A common conversation I have in clinic is around the potential benefits and risks of steroid injections, often referred to as cortisone. It actually seems to be quite divisive: people seem to either love it or hate it, just like good old marmite. I think this is in large part due to either their previous experiences or those of family or friends, and possibly due to historic press.
If people have had an injection for a painful knee (for example), they may have had one of 3 responses: (1) no improvement (2) short term improvement (3) fantastic improvement…it cured my problem.
So why the varied responses? Well, this can be due to a number of reasons. Firstly, was the injection accurately placed? We know that the more accurate an injection is, the more likely people are to have a good response. However, even a well-administered injection may not provide any benefit if it is not the most appropriate treatment for the condition. Broadly speaking, steroid injections work best in a local inflammatory situation, so if there is no inflammation it is less likely to work. Sometimes people have a short period of pain relief following injection for pain to return thereafter. In this instance, it could be due to failure to address an underlying cause for the inflammation.
The other, justifiably, talked about issue with cortisone is the potential degenerative effect it can have on joints and soft tissues. Just as steroid injections can help to remove inflammatory cells, they can also negatively impact on healthy cells such as cartilage or tendon cells. Historic studies have shown that repeat injections, often of quite high doses, can contribute to the development of joint problems such as arthritis, and in weakening of tendons. These days, contemporary practice limits both the dose per injection and the total number of injections permitted.
So where does this leave us now? Do we still inject cortisone? Well…yes! It does still have a place in many situations. It is a great treatment for lots of conditions if used appropriately such as Frozen Shoulder, tendon sheath problems of the wrist and hand, and even within joints. For some people with severe inflammatory joint or soft tissue pain, often there is nothing better at providing some welcome relief than a steroid injection.

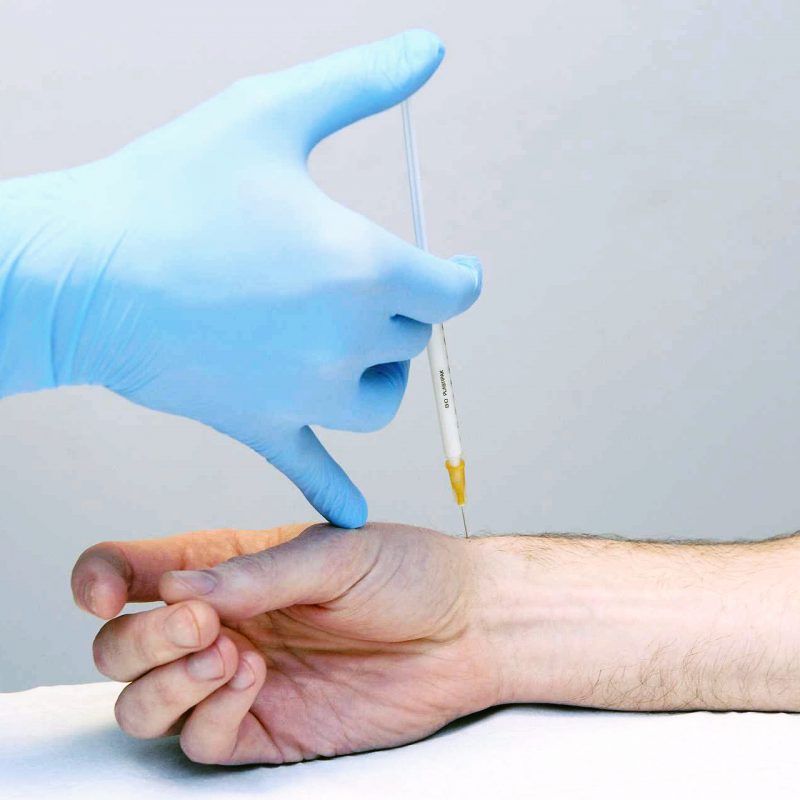
I will state my bias: in my opinion, ultrasound scanning
does offer exceptional value when it comes to injections. Firstly, it can really help us establish if
there is active inflammation, and therefore if steroid is indicated. It gives us lots of other useful information
about tendons, ligaments, bones and soft tissues which can help build a more complete picture of the problem. Furthermore, injections can be performed ‘ultrasound-guided’, meaning that the needle is visualised directly to steer it towards the target with precision accuracy.
But is it the only injection option? Not at all. There are
lots of alternatives available, however, for a number of situations I am becoming increasingly optimistic about the use of something called hyaluronic acid (Ostenil). This is a lubricating injection which is most commonly used in joints for osteoarthritis but can be used in tendon conditions too. It is far less abrasive than cortisone and therefore has far fewer side effects (least of all no unwanted degenerative effects), and also appears to provide lasting relief for a lot of people, much longer that steroid injections. If used in the correct circumstances then it can provide lasting relief for many people, especially in those with osteoarthritis.
So, in summary, cortisone injections can be both good and bad, and like any treatment it is most successful if it is appropriately matched to the condition. Ultrasound can assist in this decision-making and can also be used to improve the accuracy of the injection. When cortisone isn’t indicated there are other alternatives such as hyaluronic acid.
For more information on Injection Services at Life Fit Wellness click here.